Healthwise
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Topic Contents
- What is childhood testicular cancer?
- Types of testicular tumors
- Causes and risk factors for childhood testicular cancer
- Genetic counseling for children with testicular cancer
- Symptoms of childhood testicular cancer
- Tests to diagnose childhood testicular cancer
- Getting a second opinion
- Who treats children with testicular cancer?
- Treatment of childhood testicular cancer
- Clinical trials
- Prognosis for childhood testicular cancer
- Side effects and late effects of treatment
- Follow-up care
- Coping with your child's cancer
- Related resources
- About This PDQ Summary
Childhood Testicular Cancer (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What is childhood testicular cancer?
Testicular tumors in children can form in the tissue of one or both testicles. These tumors can be benign (not cancer) or malignant (cancerous). Benign tumors do not spread to other parts of the body. However, they may grow and press on nearby tissues, causing discomfort or other problems. Malignant tumors may spread to other parts of the body. Benign tumors are more common in young boys and infants while malignant tumors are more common in boys who have gone through puberty.
The testicles are two egg-shaped glands in the male reproductive system. They are located inside the scrotum, a sac of loose skin that lies directly below the penis. The testicles are held within the scrotum by the spermatic cord, which contains the vas deferens, vessels, and nerves of the testicles. The testicles produce male hormones, such as testosterone, and sperm.
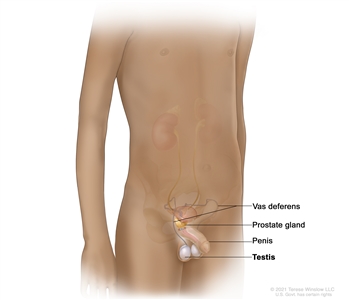
Anatomy of the male reproductive system. The male reproductive system is made up of organs and glands involved in making offspring (children). These include the vas deferens (a long tube that carries sperm out of the testes), prostate gland, penis, and testes.
Types of testicular tumors
There are two types of testicular tumors.
- Non-germ cell tumors begin in the cells that produce hormones and in the tissue that surrounds and supports the testicles. These tumors may be benign or cancerous. Types of non-germ cell tumors include:
- Juvenile granulosa cell tumors, which most often occur in young infants.
- Sertoli cell tumors, which often occur in older infants.
- Leydig cell tumors, which are more common in adolescents.
- Germ cell tumors begin in the sperm-producing cells of the testicles. Most childhood testicular tumors are germ cell tumors. Learn more about testicular germ cell tumors and their treatment at Childhood Extracranial Germ Cell Tumors Treatment.
Causes and risk factors for childhood testicular cancer
Childhood testicular cancer is caused by certain changes to the way testicular cells function, especially how they grow and divide into new cells. Often, the exact cause of these cell changes is unknown. Learn more about how cancer develops at What Is Cancer?
A risk factor is anything that increases the chance of getting a disease. Not every child with one or more of these risk factors will develop testicular cancer. And it will develop in some children who don't have a known risk factor.
The risk of testicular cancer may be increased if your child has one of the following syndromes:
- DICER1 syndrome is a disorder that may cause a goiter, polyps in the colon, and tumors of the ovary, cervix, testicle, kidney, brain, eye, and lining of the lung.
- Peutz-Jeghers syndrome is a disorder that causes polyps to form in the intestines and dark spots to form on the mouth and fingers.
- Carney syndrome or complex is a disorder that causes dark spots on the skin and tumors to form in the heart, endocrine glands, skin, and nerves.
Talk with your child's doctor if you think your child may be at risk.
Genetic counseling for children with testicular cancer
It may not be clear from the family medical history whether a child with testicular cancer has an inherited condition that increased their risk. Genetic counseling before genetic testing can help assess your child's risk of having a gene change that caused your child's tumor and whether genetic testing is needed. Genetic testing may help explain why a child develops a rare cancer or a cancer that is usually seen in adults, such as testicular cancer. Genetic counselors and other specially trained health professionals can discuss your child's diagnosis and your family's medical history to help you understand:
- the options for DICER1 gene testing
- the risk of other cancers for your child
- the risk of testicular cancer and other cancers for your child's siblings
- the risks and benefits of learning genetic information
Genetic counselors can also help you cope with your child's genetic testing results, including how to discuss the results with family members. They can advise you about whether other members of your family should receive genetic testing.
Learn more about Genetic Testing for Inherited Cancer Risk.
Symptoms of childhood testicular cancer
Children may not have symptoms of testicular cancer until the tumor has grown bigger. It's important to check with your child's doctor if your child has:
- a painless lump in the testicles
- early signs of puberty
- enlarged breasts
These symptoms may be caused by problems other than childhood testicular cancer. The only way to know is to see your child's doctor.
Tests to diagnose childhood testicular cancer
If your child has symptoms that suggest testicular cancer, the doctor will need to find out if these are due to cancer or another problem. The doctor will ask when the symptoms started and how often your child has been having them. They will also ask about your child's personal and family medical history and do a physical exam. Depending on these results, they may recommend other tests. If your child is diagnosed with testicular cancer, the results of these tests will help you and your child's doctor plan treatment.
The tests and procedures used to diagnose testicular cancer may include:
Ultrasound exam
An ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
CT scan (CAT scan)
A CT scan uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the chest, abdomen, or pelvis. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.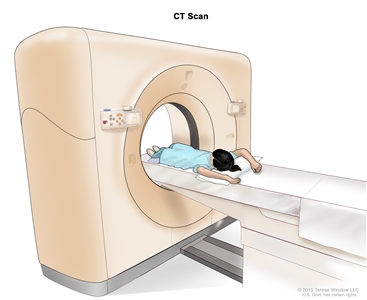
Computed tomography (CT) scan. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of areas inside the body.
Magnetic resonance imaging (MRI)
MRI uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas of the body, such as the chest, abdomen, or pelvis. This procedure is also called nuclear magnetic resonance imaging (NMRI).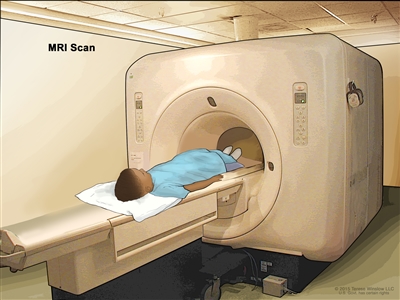
Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged.
Chest x-ray
An x-ray is a type of radiation that can go through the body and make pictures. A chest x-ray makes pictures of the organs and bones inside the chest.
Biopsy
A biopsy is a procedure in which a sample of tissue is removed from the tumor so that a pathologist can view it under a microscope to check for signs of cancer.
Serum tumor marker test
A serum tumor marker test examines a sample of blood to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. If an increased level of the tumor marker alpha-fetoprotein is found in the blood, it means the patient has a testicular germ cell tumor, not a testicular non-germ cell tumor.
DICER1 genetic testing
DICER1 genetic testing examines a sample of blood or saliva for changes in the DICER1 gene.
Getting a second opinion
You may want to get a second opinion to confirm your child's testicular cancer diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the genetic test results, pathology report, slides, and scans. This doctor may agree with the first doctor, suggest changes to the treatment plan, or provide more information about your child's cancer.
To learn more about choosing a doctor and getting a second opinion, see Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital that can provide a second opinion. For questions you might want to ask at your child's appointments, see Questions to Ask Your Doctor about Cancer.
Who treats children with testicular cancer?
A pediatric oncologist, a doctor who specializes in treating children with cancer, oversees treatment for testicular cancer. The pediatric oncologist works with other health care providers who are experts in treating children with cancer and who specialize in certain areas of medicine. Other specialists may include:
- pediatrician
- pediatric surgeon
- pediatric urologist
- pathologist
- pediatric nurse specialist
- rehabilitation specialist
- social worker
- psychologist
- fertility specialist
Treatment of childhood testicular cancer
There are different types of treatment for children and adolescents with testicular cancer. You and your child's cancer care team will work together to decide treatment. Many factors will be considered, such as your child's overall health and whether the cancer is newly diagnosed or has come back.
Your child's treatment plan will include information about the cancer, the goals of treatment, treatment options, and the possible side effects. It will be helpful to talk with your child's cancer care team before treatment begins about what to expect. For help every step of the way, see our booklet, Children with Cancer: A Guide for Parents.
Treatment for non-germ cell testicular cancer in children is usually surgery to remove the tumor. In some cases, the entire testicle with cancer may need to be removed.
If the cancer comes back after treatment, your child's doctor will talk with you about what to expect and possible next steps. There may be treatment options to shrink the cancer or control its growth. If there are no treatment options, your child can receive care to control symptoms from cancer so they can be as comfortable as possible.
Clinical trials
For some children, joining a clinical trial may be an option. There are different types of clinical trials for childhood cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your child's age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Prognosis for childhood testicular cancer
If your child has been diagnosed with testicular cancer, you likely have questions about how serious the cancer is and your child's chances of survival. The likely outcome or course of a disease is called prognosis. In children, the prognosis for testicular cancer is usually excellent after surgery to remove the tumor.
Side effects and late effects of treatment
Cancer treatments can cause side effects. Which side effects your child might have depends on the type of treatment they receive, the dose, and how their body reacts. Talk with your child's treatment team about which side effects to look for and ways to manage them.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Problems from cancer treatment that begin 6 months or later after treatment and continue for months or years are called late effects. Physical problems, such as problems with fertility, are a late effect of treatment.
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the possible late effects caused by some treatments. Learn more about Late Effects of Treatment for Childhood Cancer.
Follow-up care
As your child goes through treatment, they will have follow-up tests or check-ups. Some of the tests that were done to diagnose the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has recurred (come back).
Coping with your child's cancer
When a child has cancer, every member of the family needs support. Taking care of yourself during this difficult time is important. Reach out to your child's treatment team and to people in your family and community for support. To learn more, see Support for Families: Childhood Cancer and the booklet Children with Cancer: A Guide for Parents.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood testicular cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Testicular Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/testicular/patient/child-testicular-treatment-pdq. Accessed <MM/DD/YYYY>.
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2024-10-10
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.



